Discussion
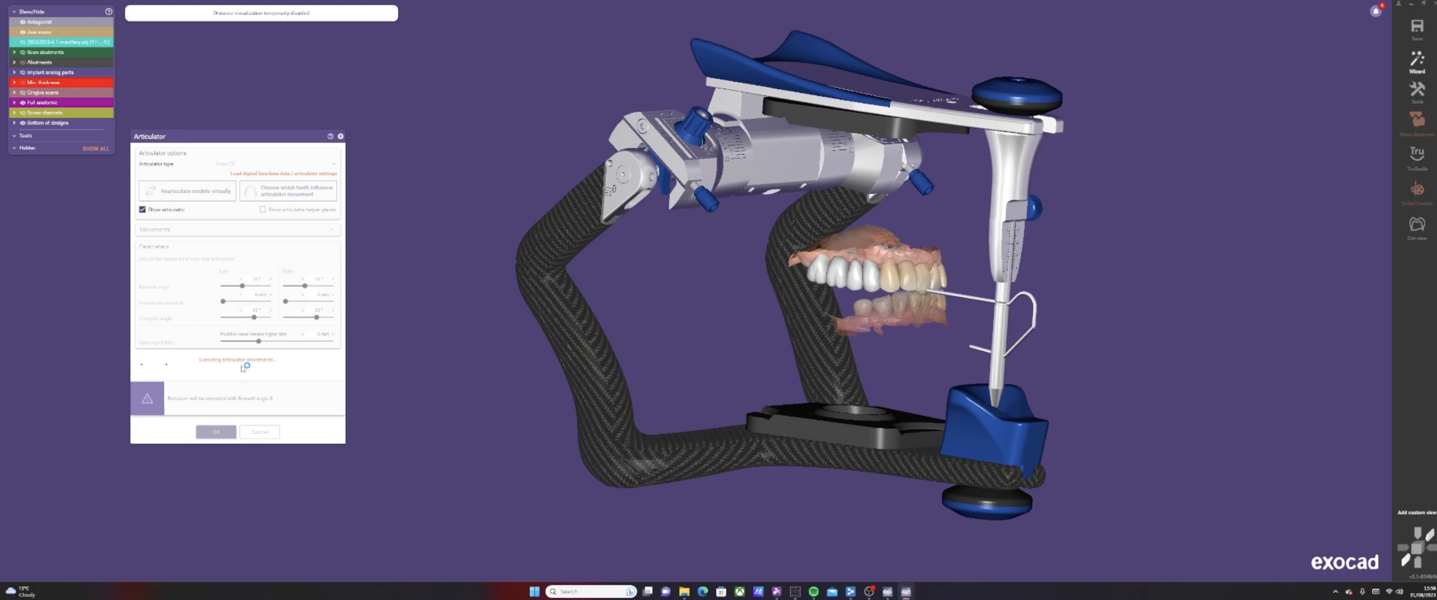
The integration of digital dentistry into clinical practice has been a transformative evolution in the field. The case presented here underscores the importance of a comprehensive digital workflow in modern implant dentistry. The use of virtual planning, guided surgery and in-house milling ensured precision and reduced the overall treatment time.
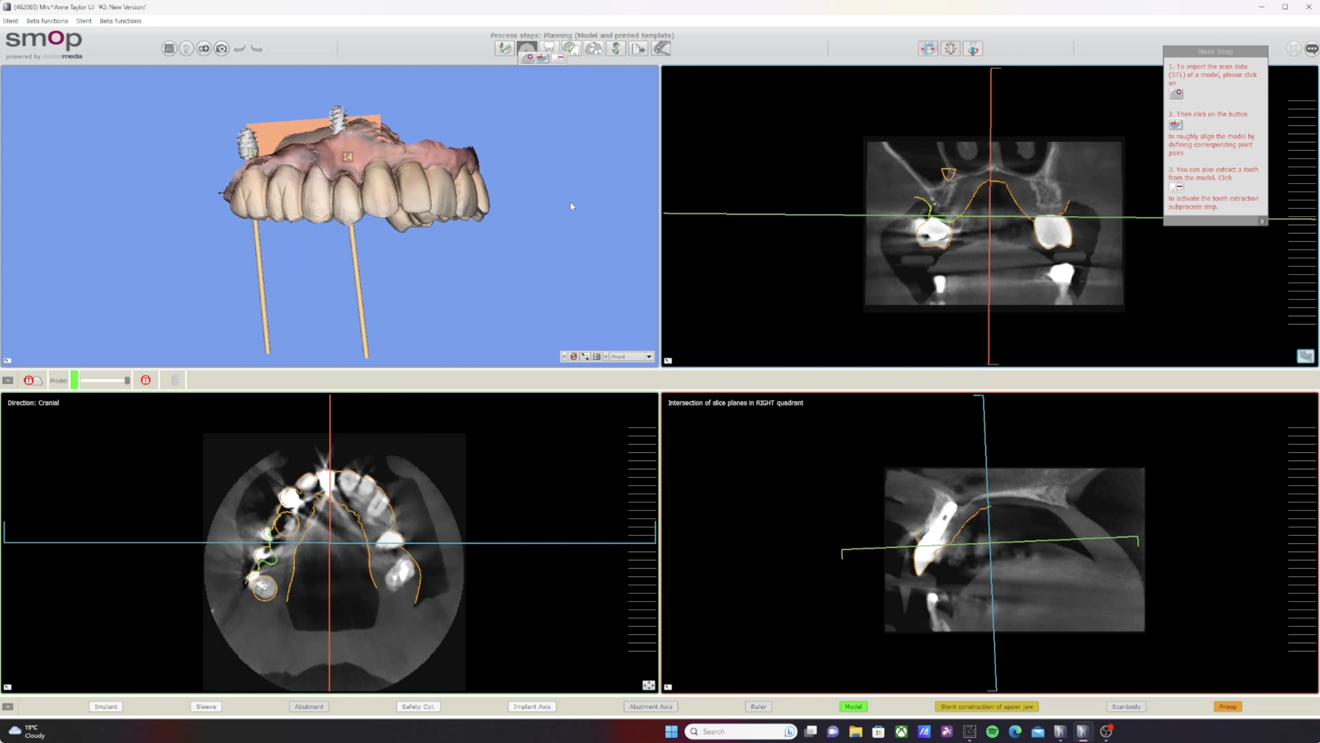
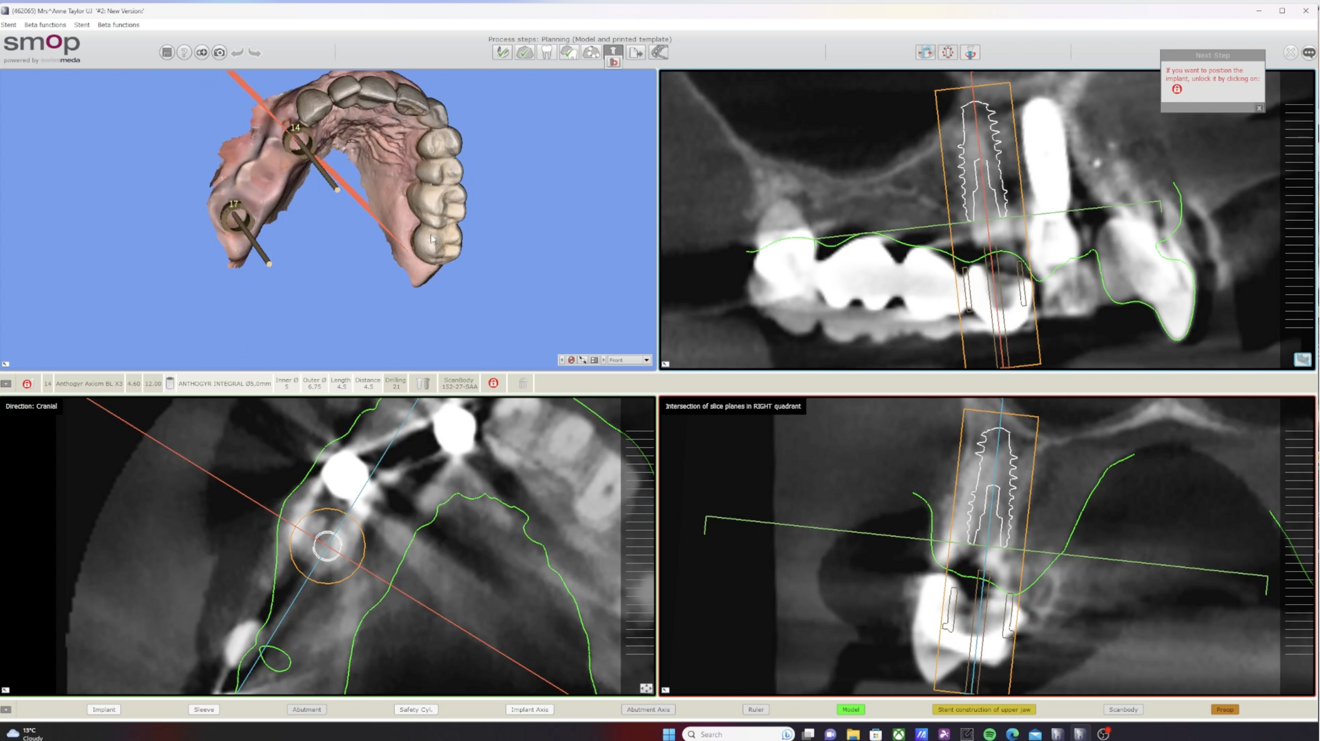
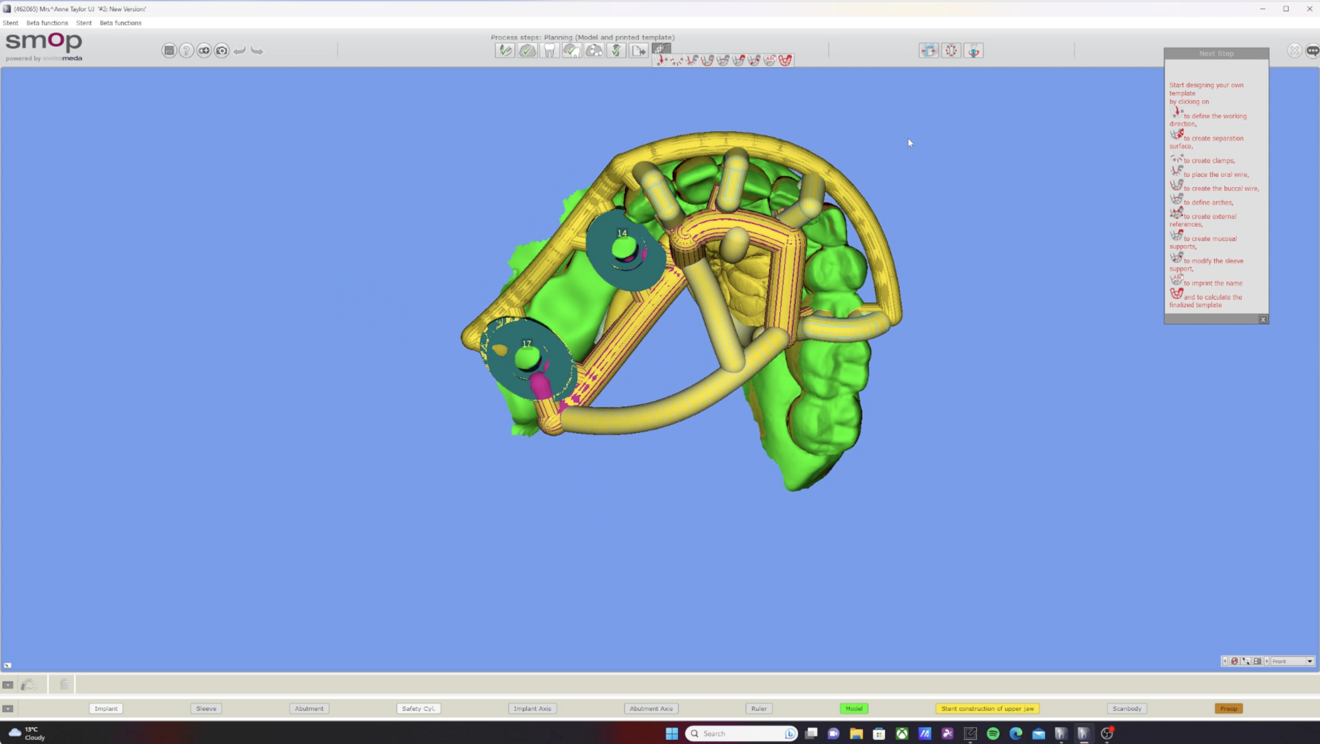
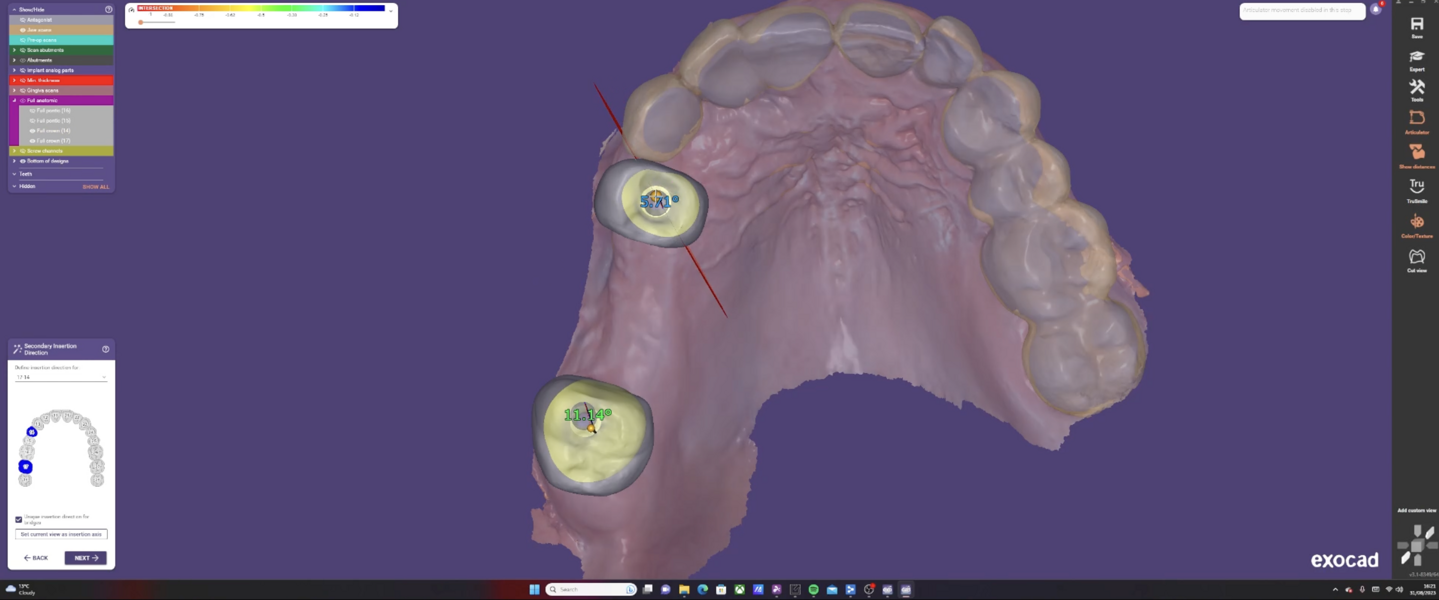
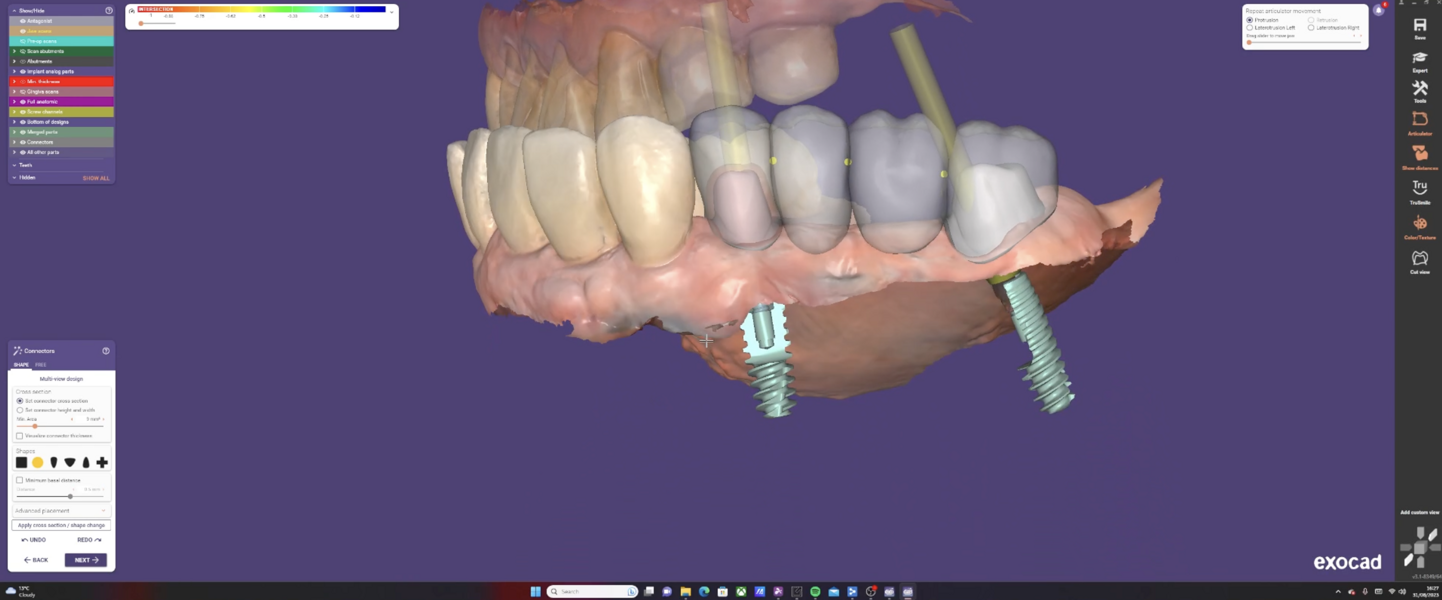
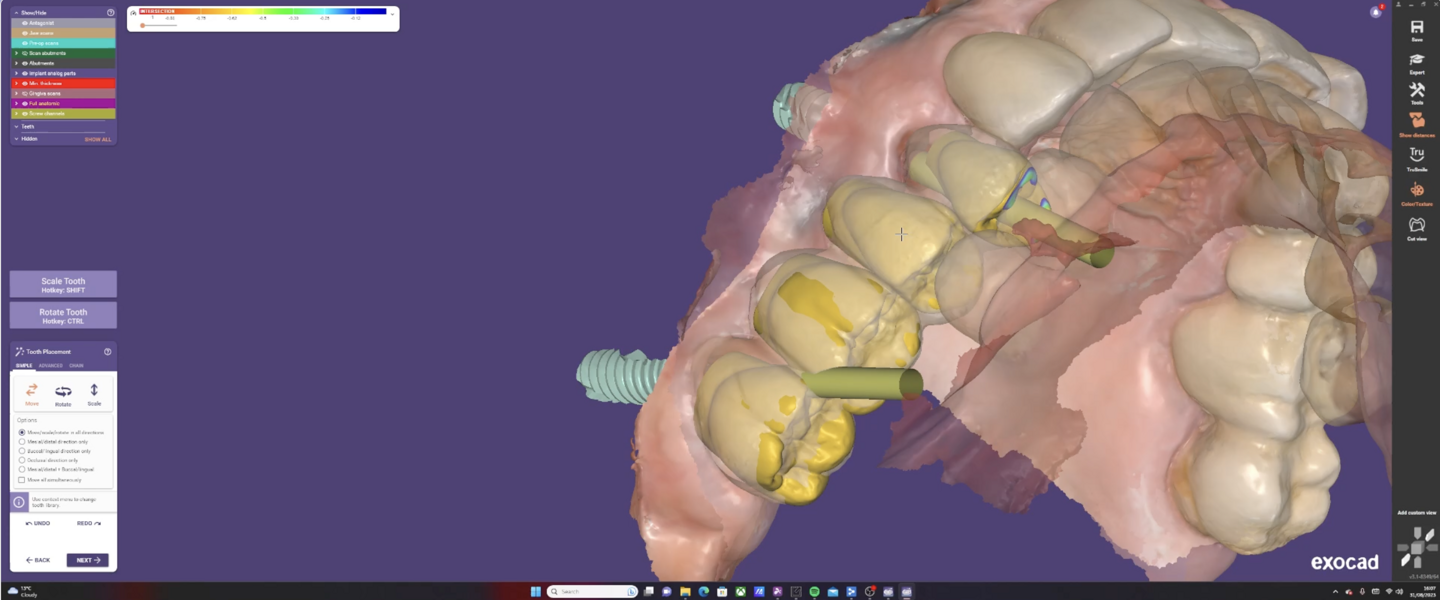
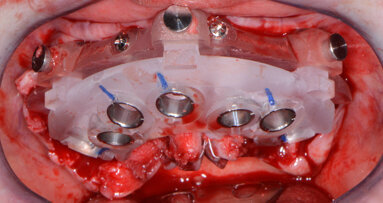
Virtual planning and guided surgery
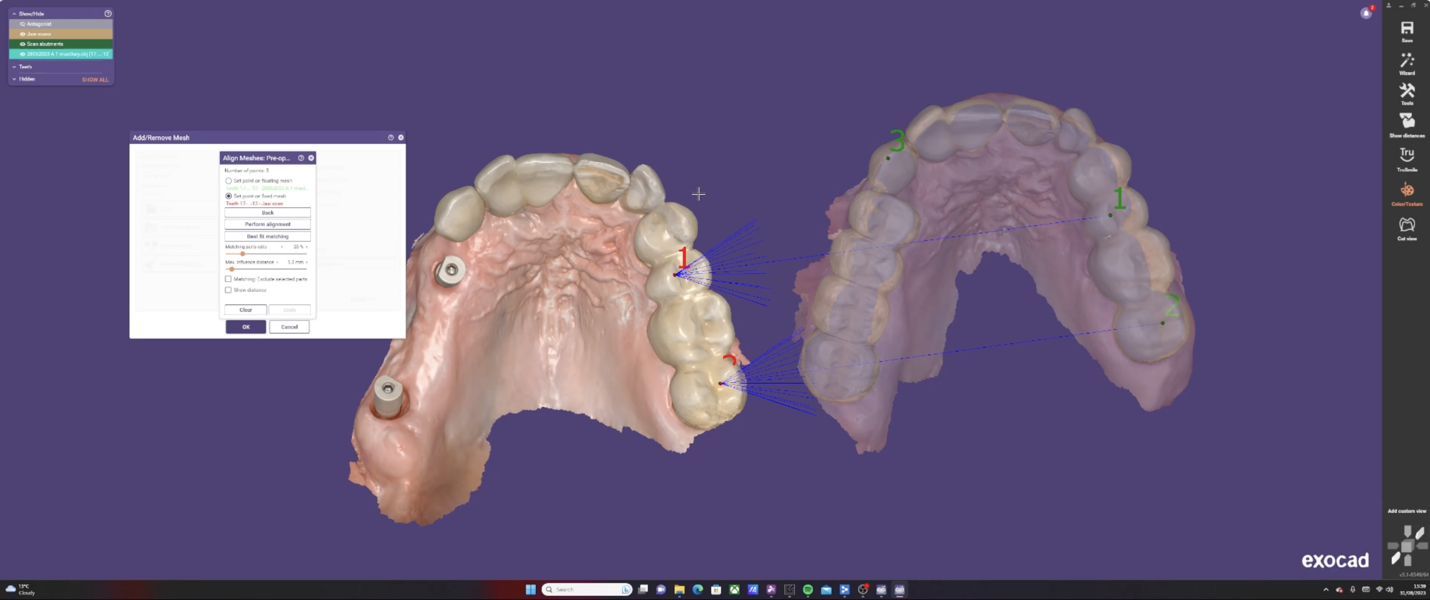
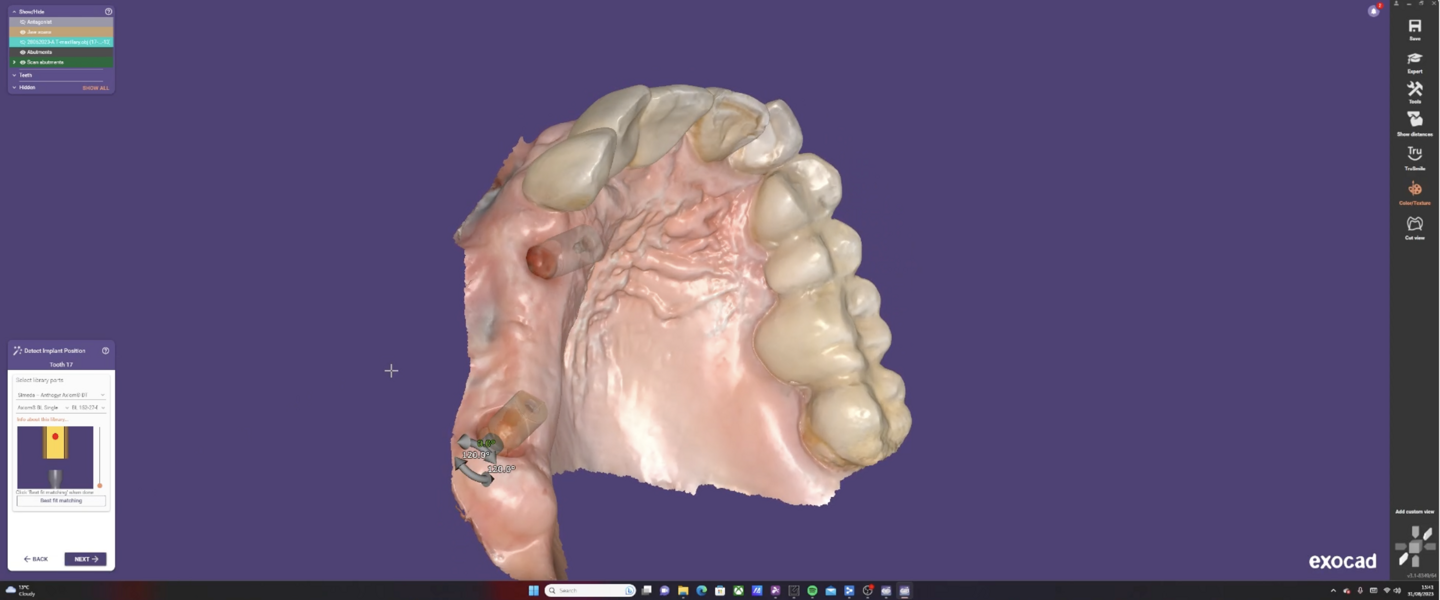
The utilisation of virtual planning tools, such as Medit Design and SMOP, allows for a more predictable surgical outcome. Mangano et al. highlight that digital workflows, including virtual planning and guided surgery, improve the accuracy of implant placement, reduce surgical time and minimise postoperative complications.1 This precision ensures that the implant is placed in the most optimal position, reducing the risk of complications and ensuring the longevity of the implant.
Immediate implant placement
Immediate implant placement, as executed in this case, has its advantages. Chen and Buser emphasise the benefits of immediate implant placement, including reduced treatment time, preservation of soft and hard tissue, and improved aesthetic outcomes.2 This method not only speeds up the treatment process but also results in greater patient satisfaction owing to the reduced number of visits and faster recovery.
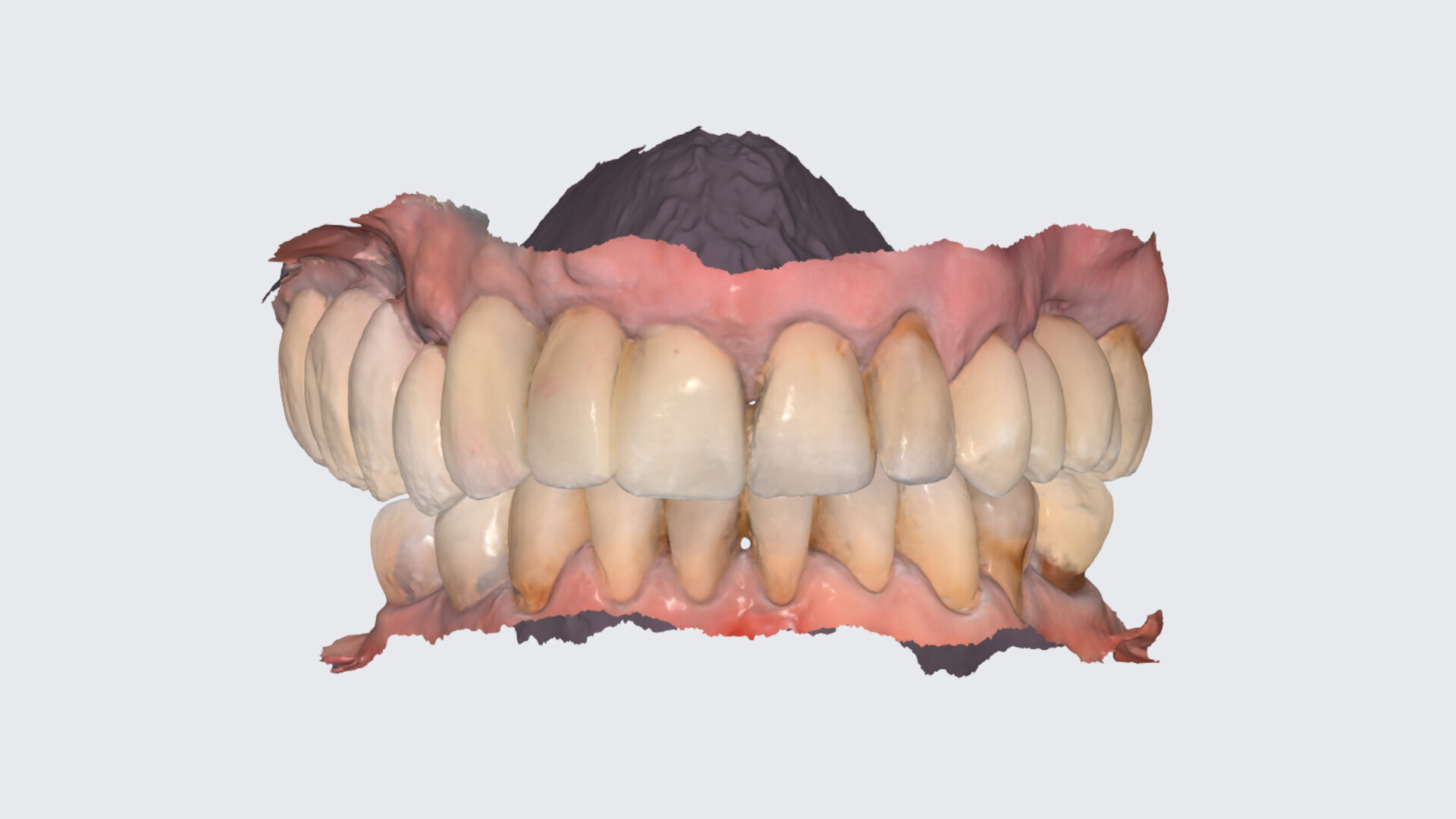
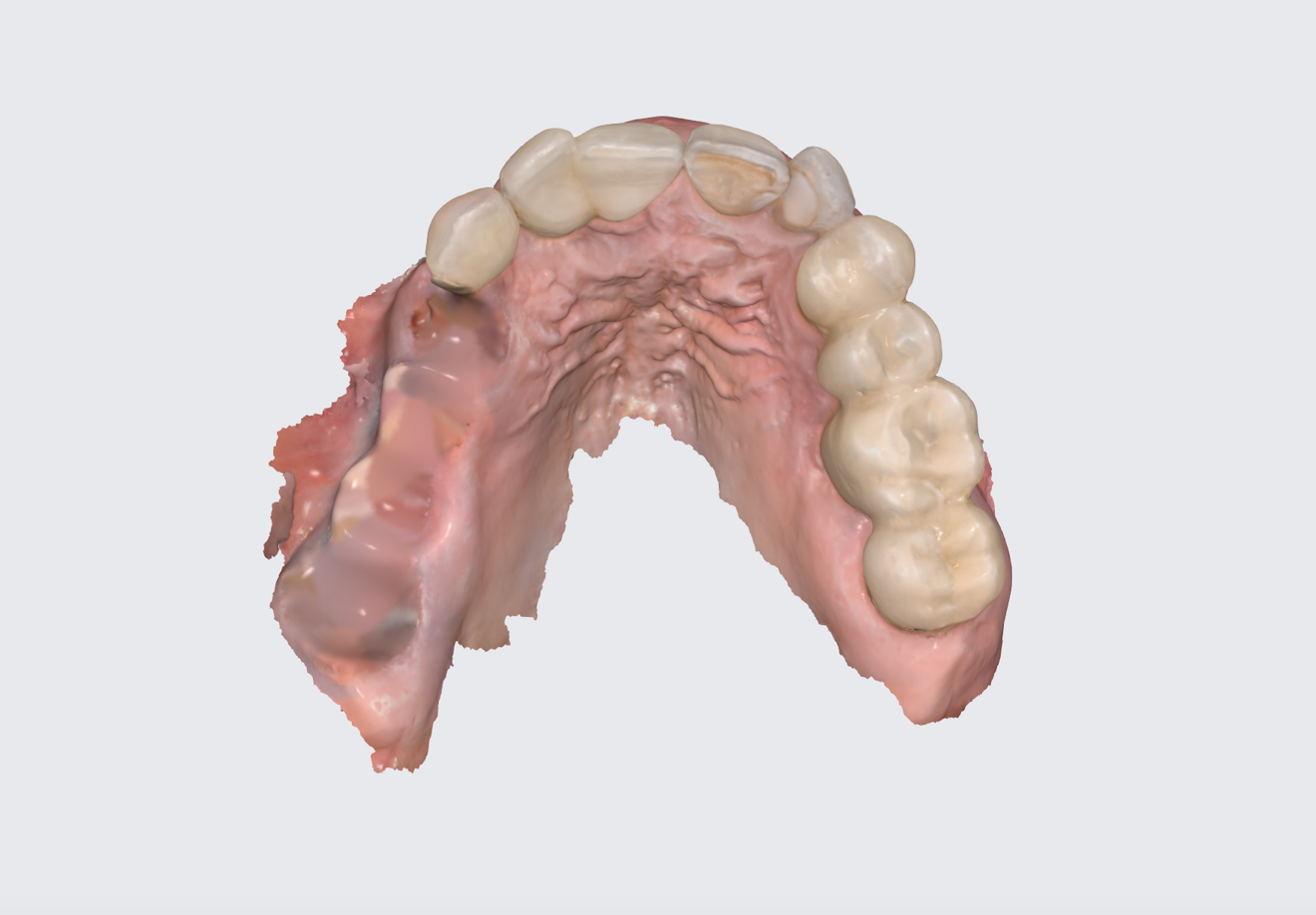
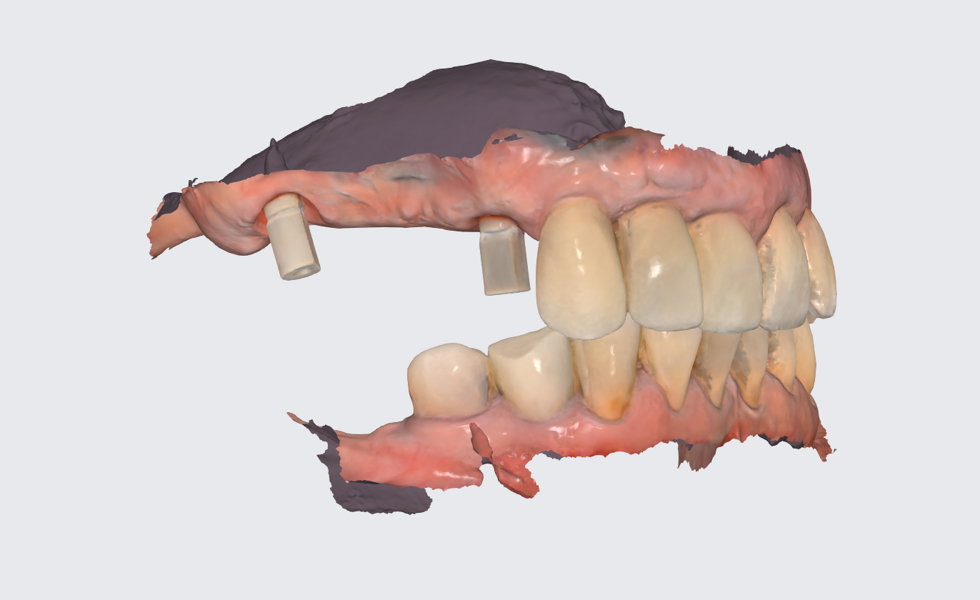
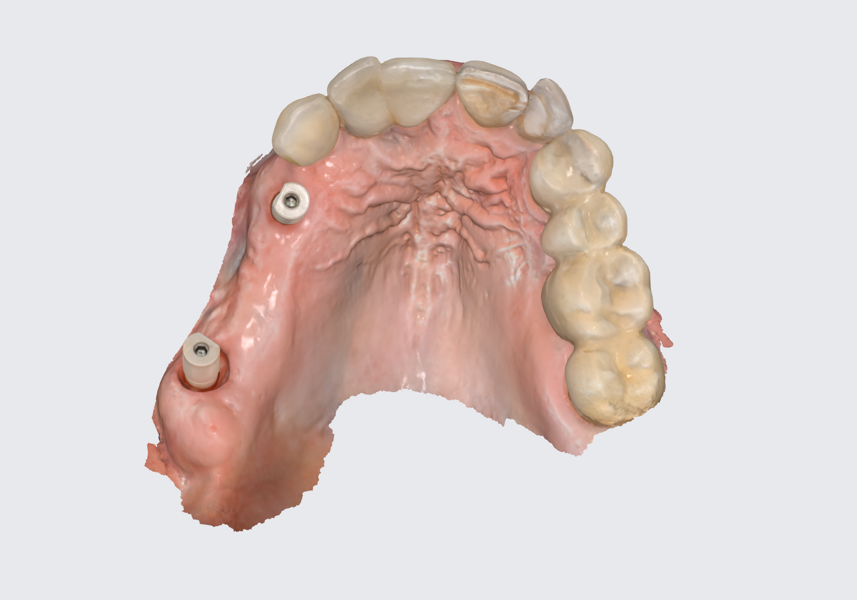
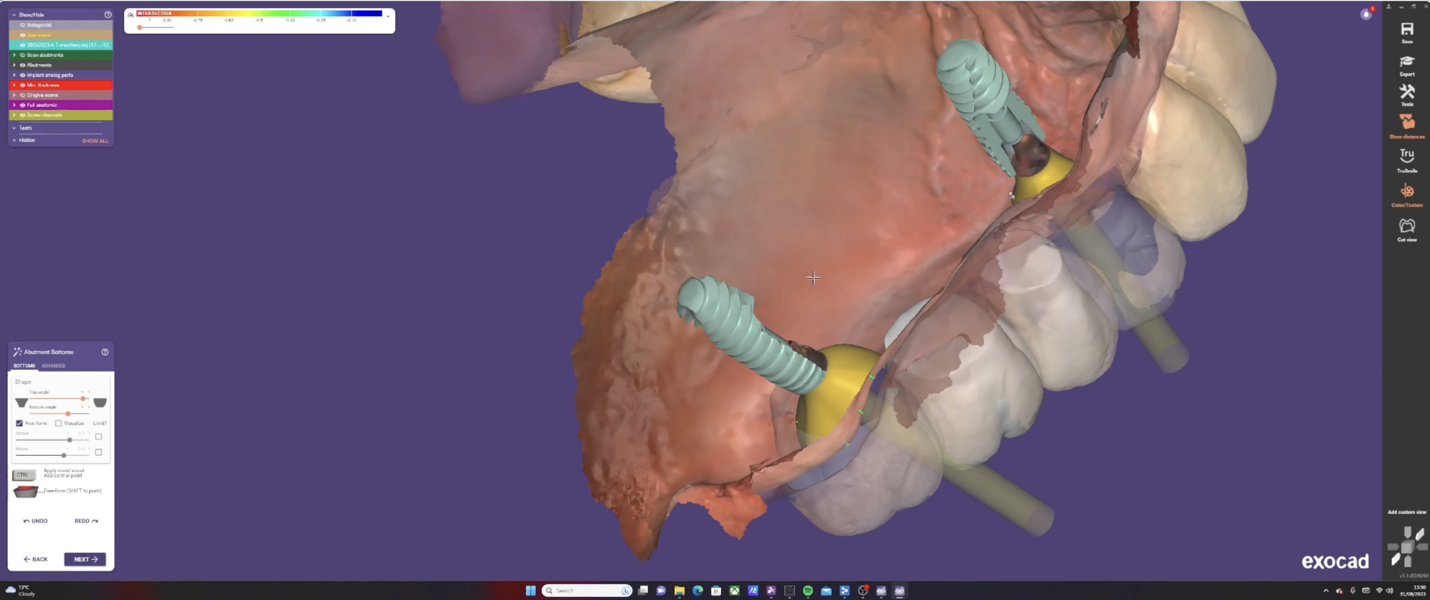
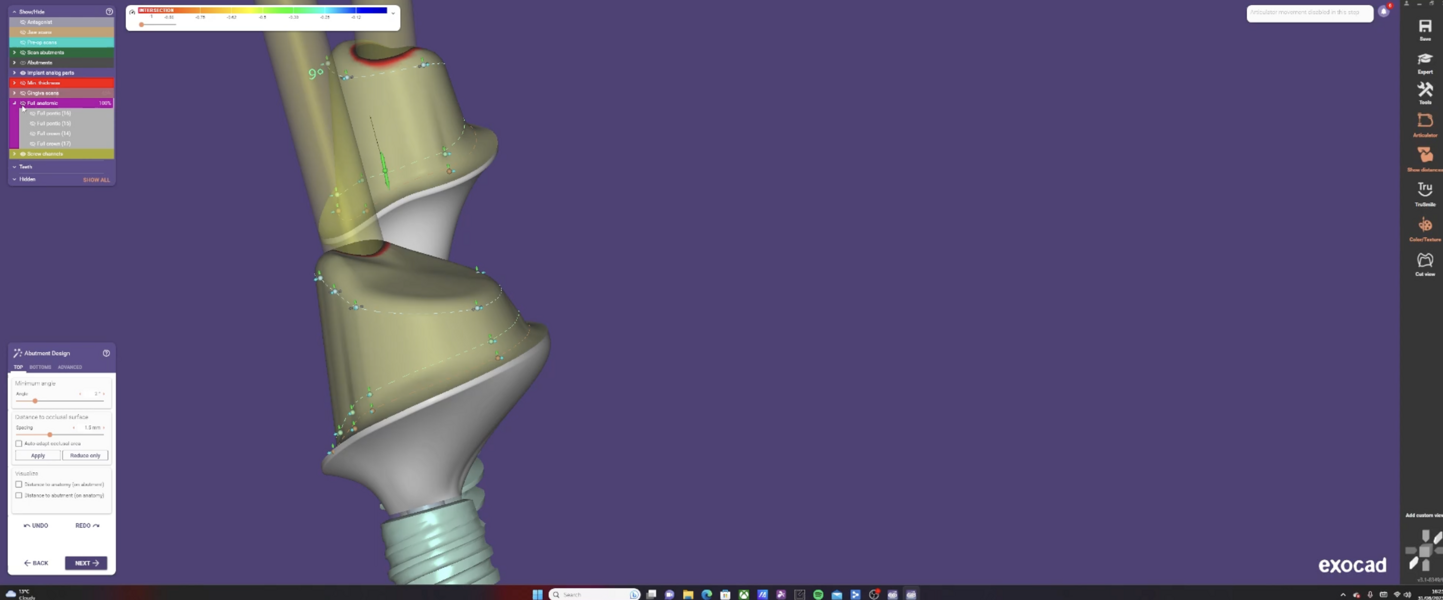
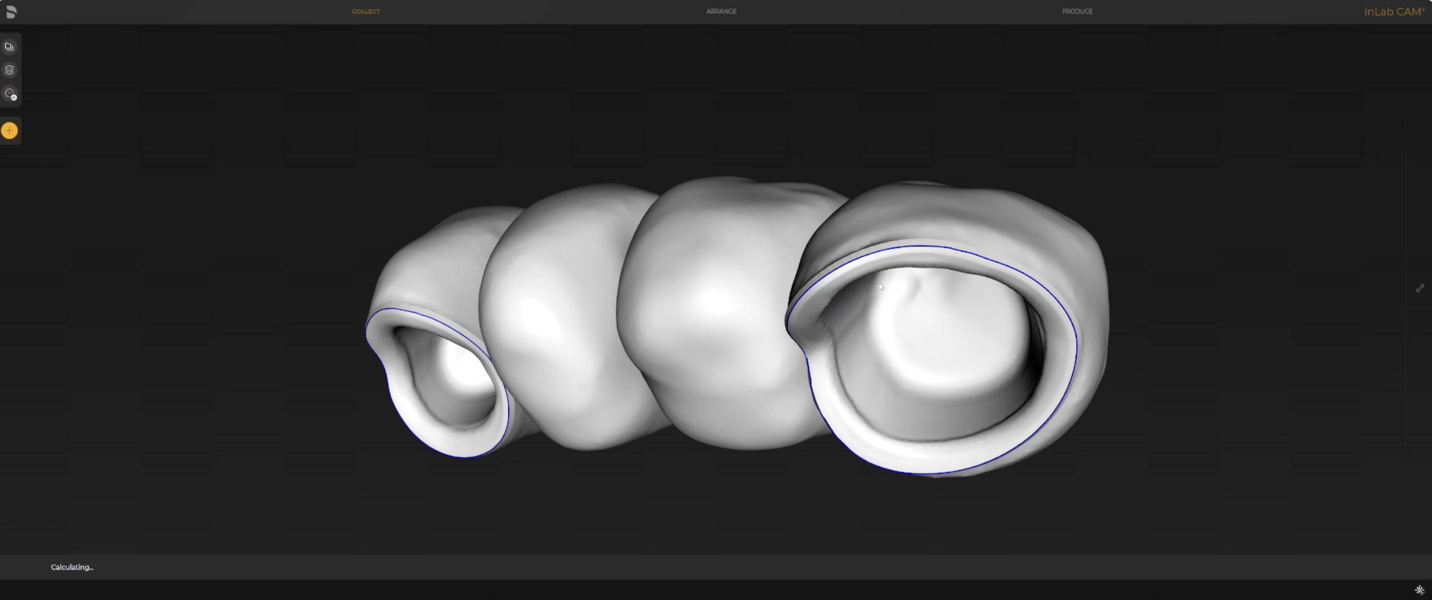
Digital impressions and in-house milling
The Medit i700 scanner was instrumental in obtaining accurate digital impressions. According to Nulty, the trueness and precision of digital scanners, including the Medit i700, are remarkable, ensuring that the final prosthesis fits perfectly.3 Furthermore, in-house milling, as done in this case, provides the clinician with greater control over the design and fit of the final prosthesis, leading to improved patient satisfaction.4
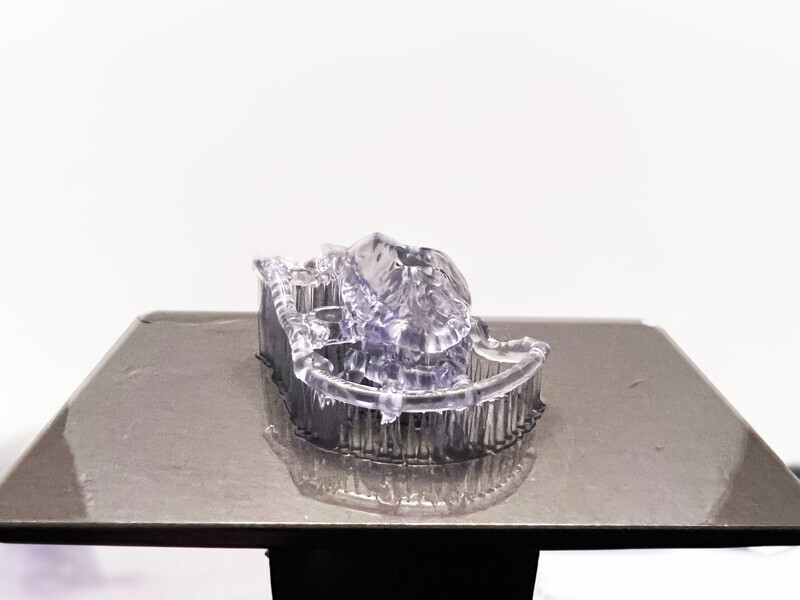
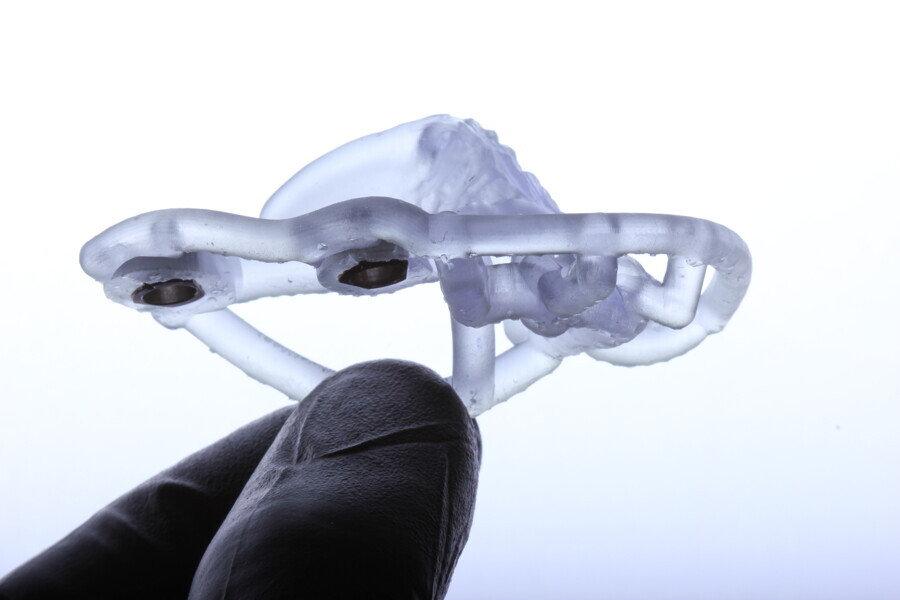
3D printing and accuracy
Nulty compared the trueness and precision of various 3D printers, including the MAX UV, and found them to be highly accurate.5 The MAX UV was statistically superior to the others, having an overall trueness of under 35 μm, ensuring that the printed surgical guides fit precisely during surgery.5 The accuracy of such printers is crucial in ensuring that the surgical guide aligns perfectly with the patient’s anatomy, supporting successful implant placement.
Material selection
The choice of bovine xenograft for socket augmentation is supported by studies that have shown its efficacy in preserving alveolar ridge dimensions after extraction.6 Additionally, the use of lithium disilicate, known for its excellent aesthetic properties and durability, for the final bridge aligns with the current trend in restorative dentistry.7
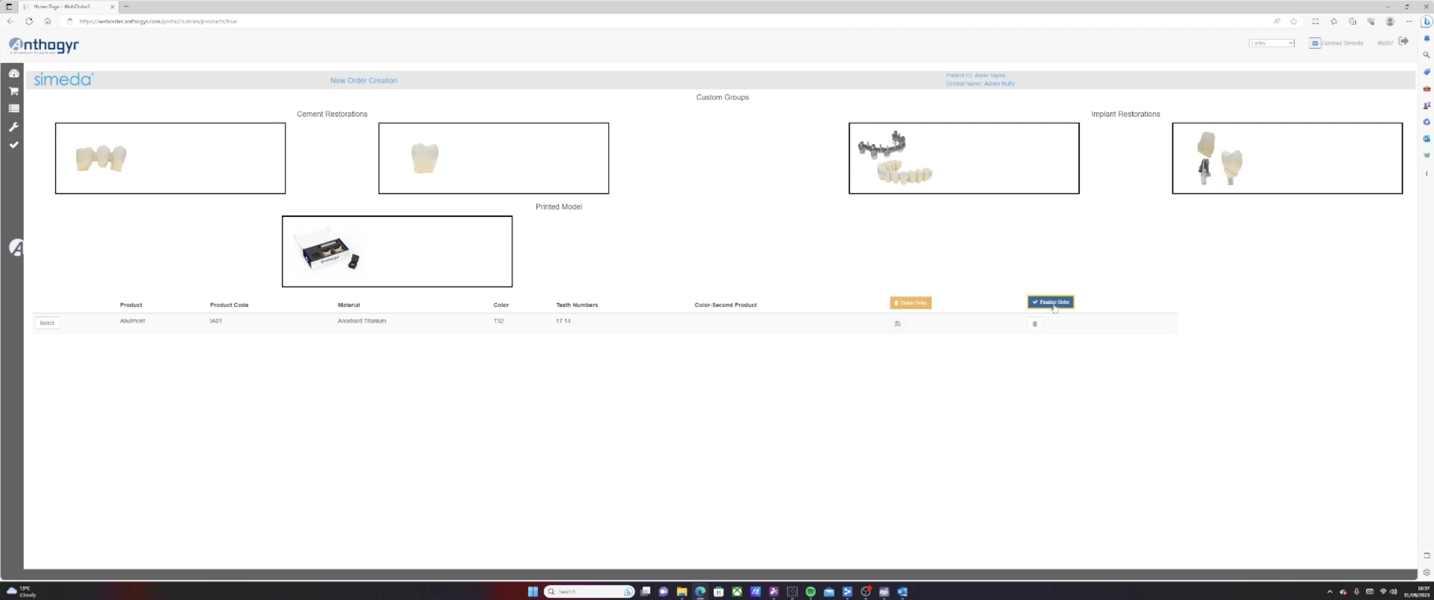
Collaborative approach
Collaboration between different digital tools, materials and experts, as seen in this case, is a testament to the multidisciplinary nature of modern dentistry. Such an approach ensures that patients receive the best possible care, combining expertise from various domains.
Primary stability and implant design
One of the critical aspects of successful dental implant placement is achieving excellent primary stability. Primary stability refers to the mechanical stability of an implant immediately after placement, and it is a crucial factor in determining the success of osseointegration and the overall outcome of the implant procedure. The Axiom X3 implant, having a unique design, has been recognised for providing exceptional primary stability. Primary stability ensures that the implant securely anchors in the bone, reducing micro-movements that can hinder the osseointegration process. This stability is not just beneficial for the immediate postoperative period but also plays a pivotal role in the long-term success of the implant.8
Conclusion
Digital dentistry, when used comprehensively, can offer patients a swift and precise treatment plan, leading to predictable outcomes. This case serves as a testament to the advancements in the field and their practical applications.
In conclusion, the advancements in digital dentistry, as demonstrated in this case, offer a holistic approach to patient care. By integrating various digital tools and techniques, clinicians can achieve predictable, efficient and aesthetically pleasing outcomes.



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 International / International
International / International
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East
































































To post a reply please login or register