This rather carpenter-like approach nonetheless yielded much higher success as clinicians looked to push the envelope with ever-higher insertion torques,3 perceived as increasing primary stability, and achieved comparable survival rates to those of conventional loading protocols, at least in the short to medium term. However, the literature has since become replete with evidence that such high insertion torques, typically > 50 Ncm, are in fact damaging the surrounding bone, these high strains resulting in microfractures, loss of vascularisation, osteocyte cell death and consequently waves of resorption propagating at some distance from the bone-to-implant interface.4–6 At the extreme, this has resulted in excessive marginal bone loss and ultimately compression necrosis and complete implant failure.7,8 In the longer term, it has been proposed that the damage induced in the bone makes it more vulnerable to advancing marginal bone loss and peri-implantitis.9 It is known that healing and therefore osseointegration are delayed and that the resulting integration is of inferior quality, bone-to-implant contact being reduced. Thus, while it may be true that success rates for immediate loading when higher insertion torque is used are comparable to those of conventional implant loading, there remains a broad lack of knowledge about the long-term consequences arising from the damage induced in the peri-implant bone as well as the misconception that lower insertion torques yield higher failure.
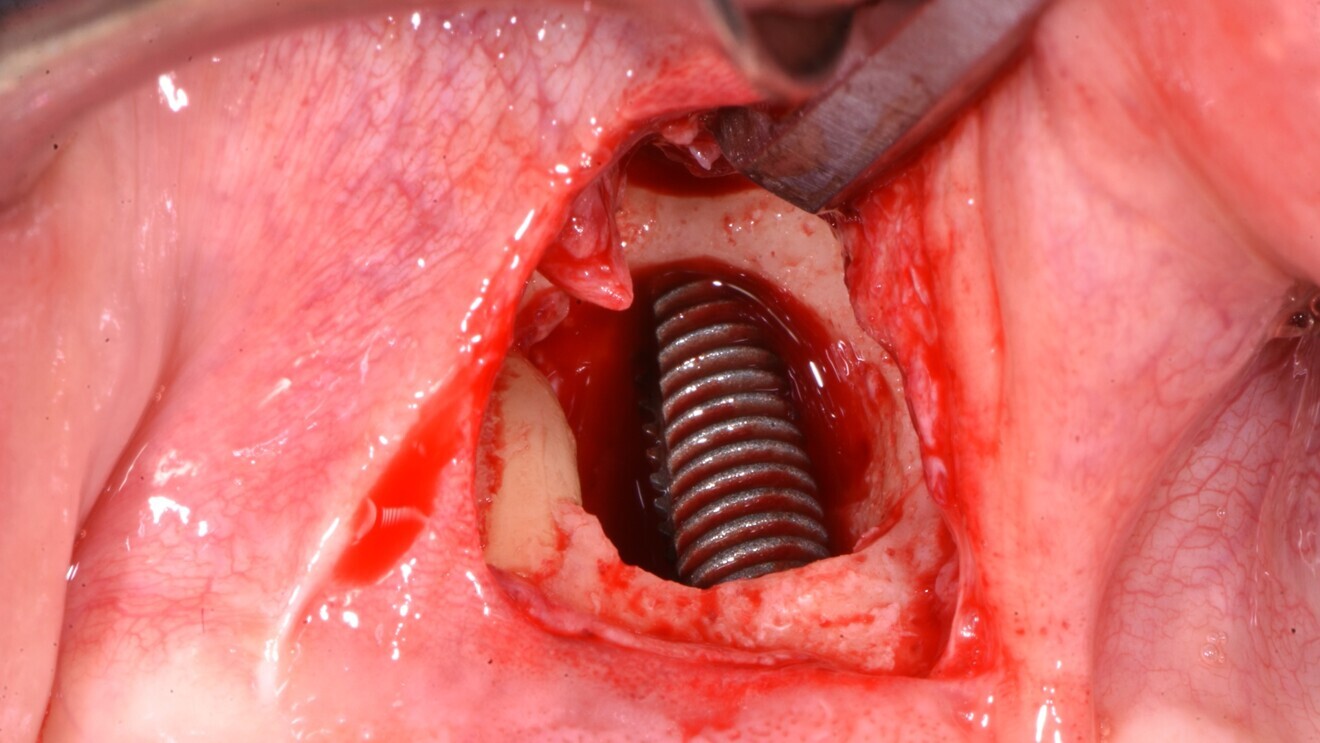
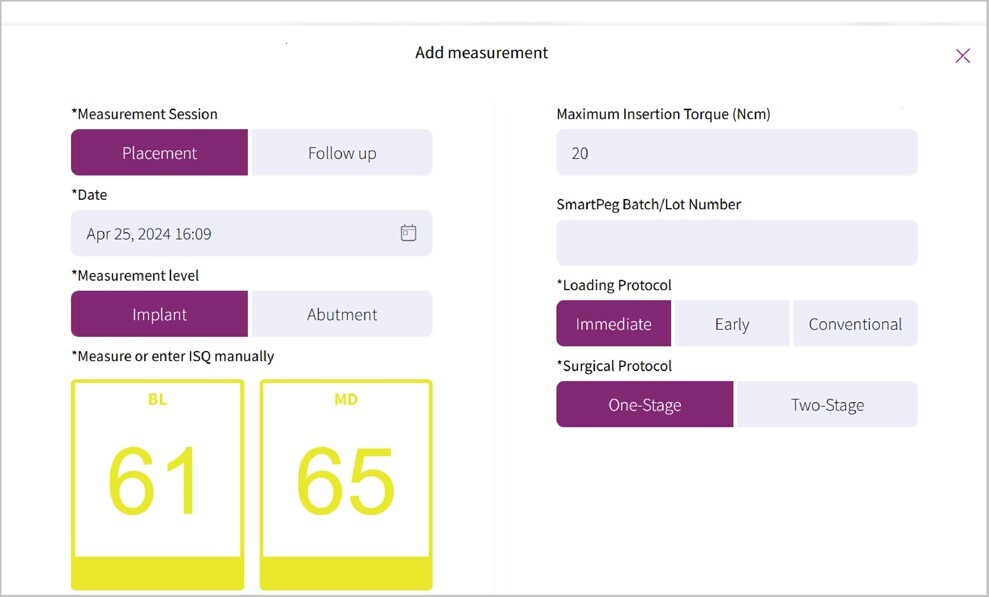
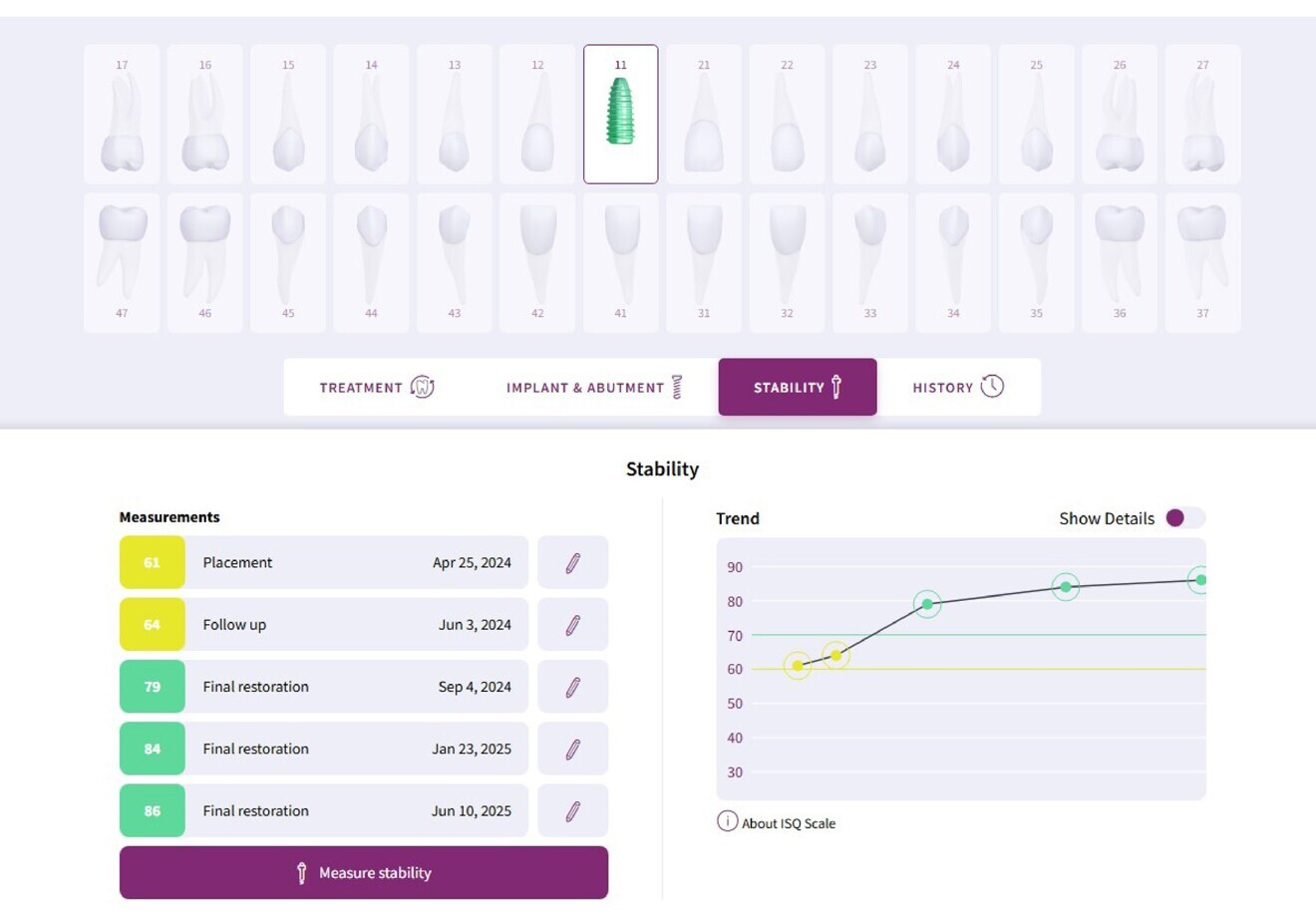
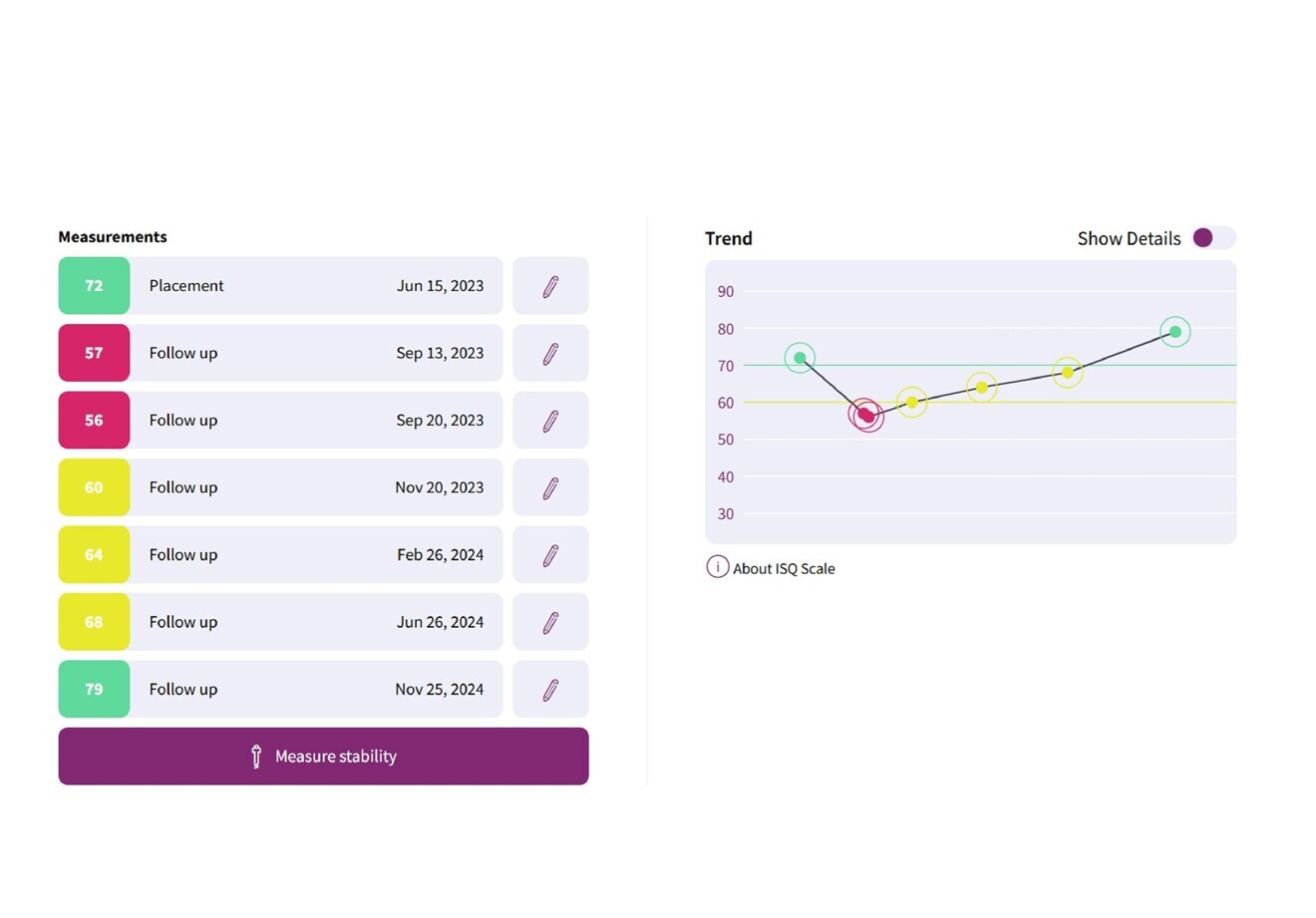
The issue is one of perception and threshold. Since many clinicians now happily use torques of 75 Ncm or more, the idea of placing an implant to 20 Ncm seems unreliable at best and high risk at worst, and there has been a complete failure to grasp the notion that 20–25 Ncm represents a likely threshold above which additional increases in torque yield little in the way of added stability, but only damage the bone. I first proposed this idea in 201110 and again discussed it in an editorial in the International Journal of Oral and Maxillofacial Implants,11 and I presented subsequent research demonstrating that baseline resonance frequency analysis (RFA) can yield implant stability quotient (ISQ) values approaching or even exceeding the desired target of 70 when using an insertion torque of ≤ 25 Ncm.12 More importantly, the singular benefit of RFA is the ability to repeat measurements over time, enabling the clinician to infer the dynamic biological changes that are taking place during healing and thus gain objective evidence of ongoing osseointegration, thereby allowing the clinician to restore the implant at the most appropriate time and with greater confidence. In contrast, insertion torque is a once-off measure and can therefore provide no longitudinal information about the dynamic process of osseointegration. The following case report is an everyday example of my own experience of placing implants into extraction sockets, followed by immediate provisionalisation, using low insertion torque and performing RFA to document the ISQ values over time.
Case report
A 37-year-old male patient was referred to my clinic for extraction and replacement of a failing maxillary right central incisor. The history revealed that the patient had suffered a childhood trauma at age 12, when the tooth was fractured close to the gingival margin. The patient underwent endodontic therapy for root canal obturation, and the tooth was crowned. After ten years, the patient became aware of symptoms, and a recurrent abscess was diagnosed. The root canal was partially filled with composite to attempt to further obturate it. After a further five years, the patient was provided with a new post and crown. Nonetheless, the infection remained, so approximately nine years before, the tooth had undergone apicoectomy, after which it settled down for a period, but it flared up again in early 2024. At that point, the patient was referred to my practice for treatment.
On examination, the patient presented with a minimally restored dentition with a few composite restorations and a crown on tooth #11. The tooth being in the aesthetic zone increased the challenge of delivering a good outcome. The patient had a healthy periodontium and only a few isolated non-pathological pockets of 4–5 mm in depth at the lingual surfaces of the mandibular molars, accompanied by some minor bleeding on probing. The patient was advised to seek more regular hygiene focusing on these areas.
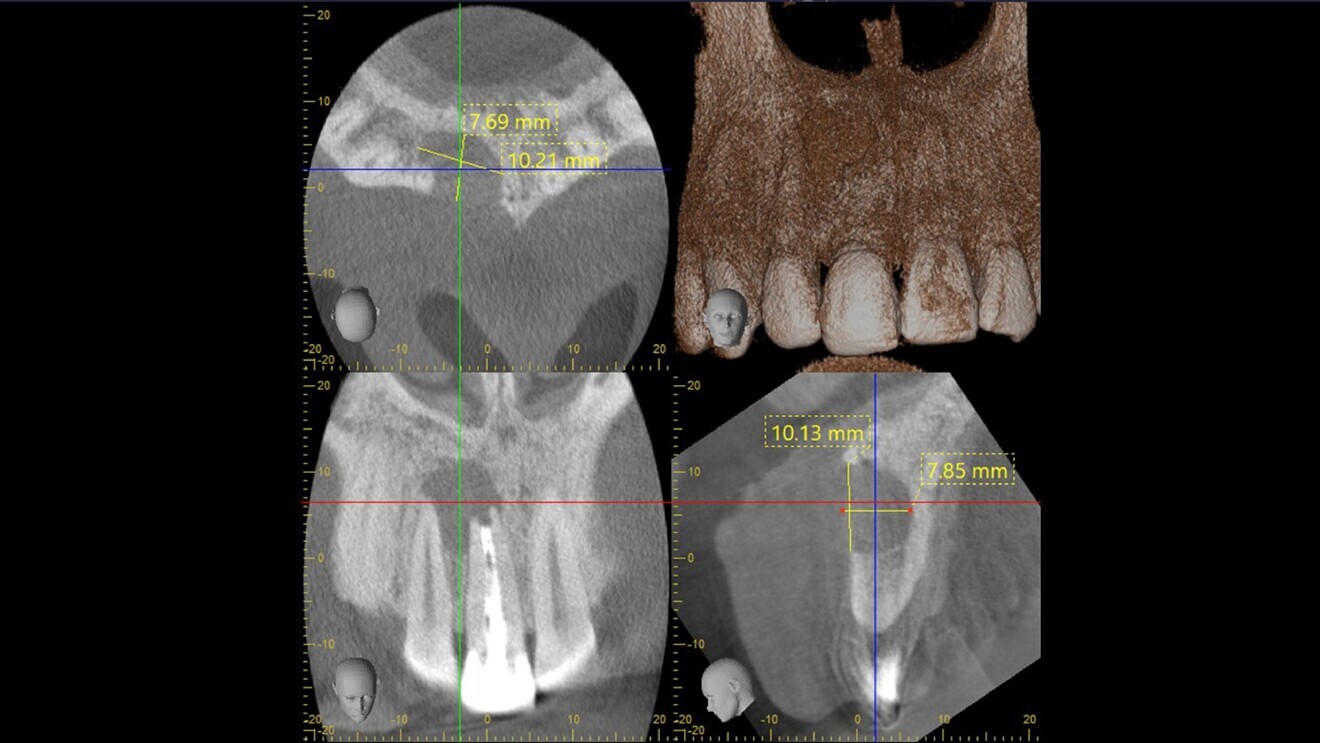
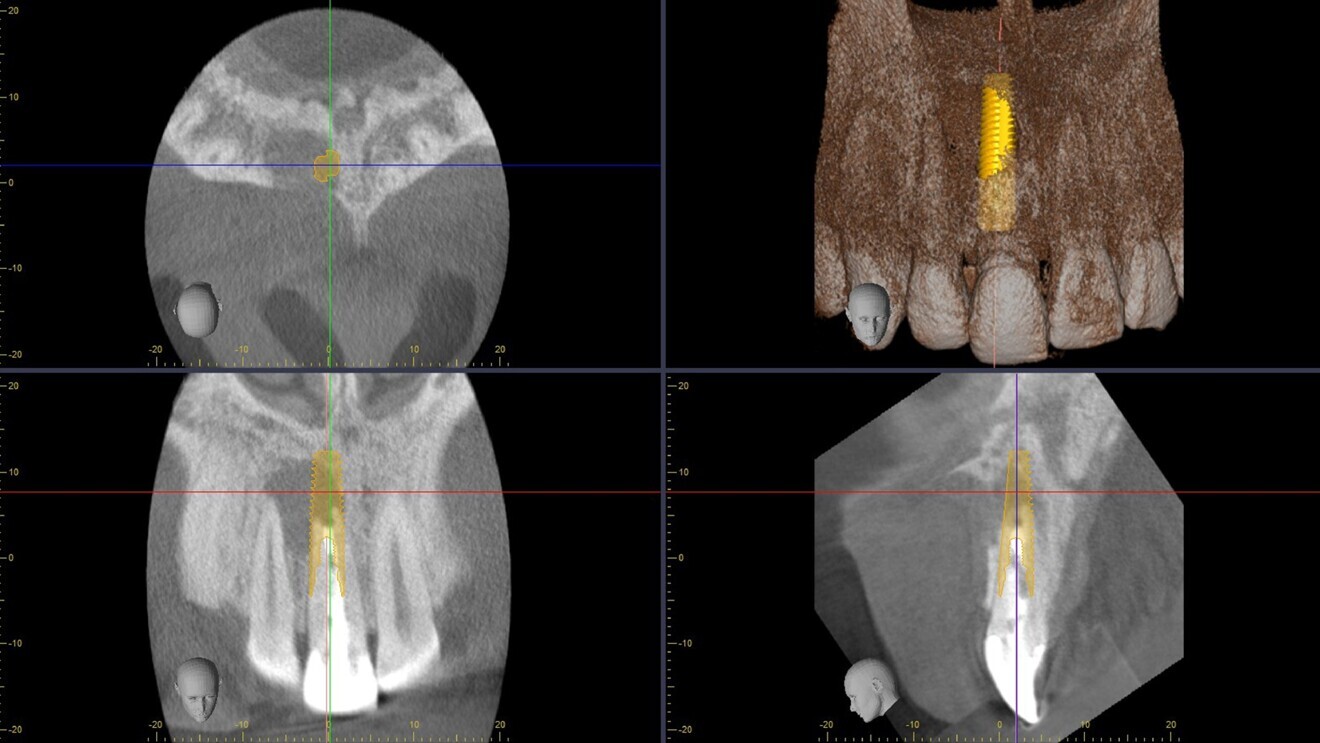
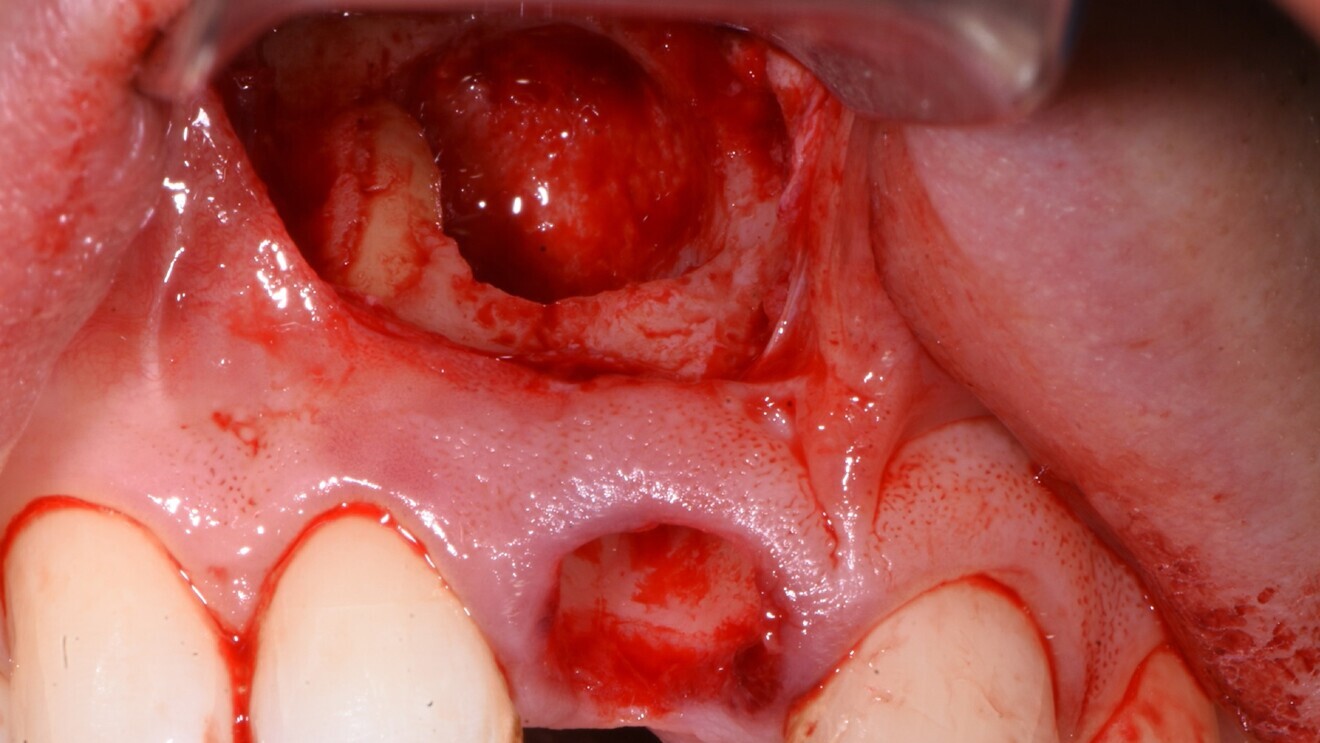
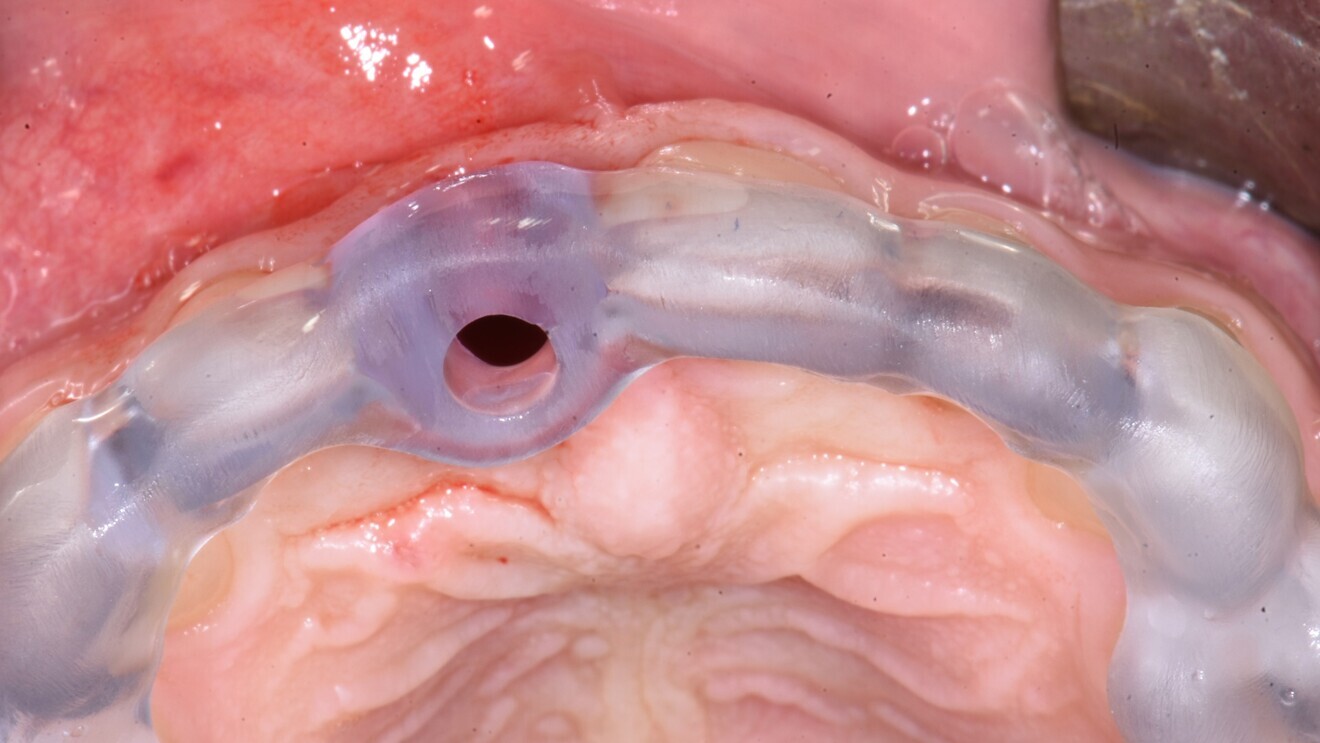
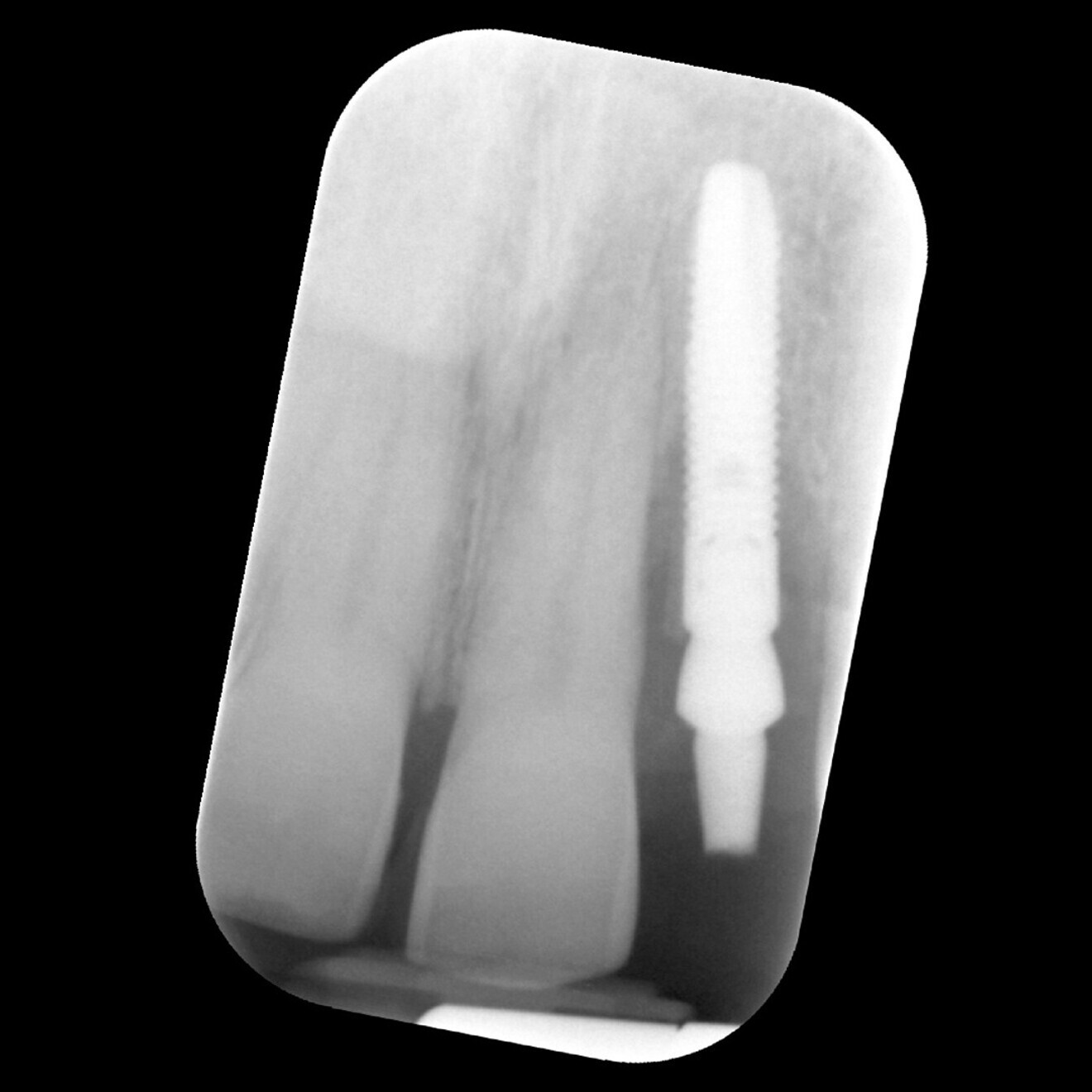
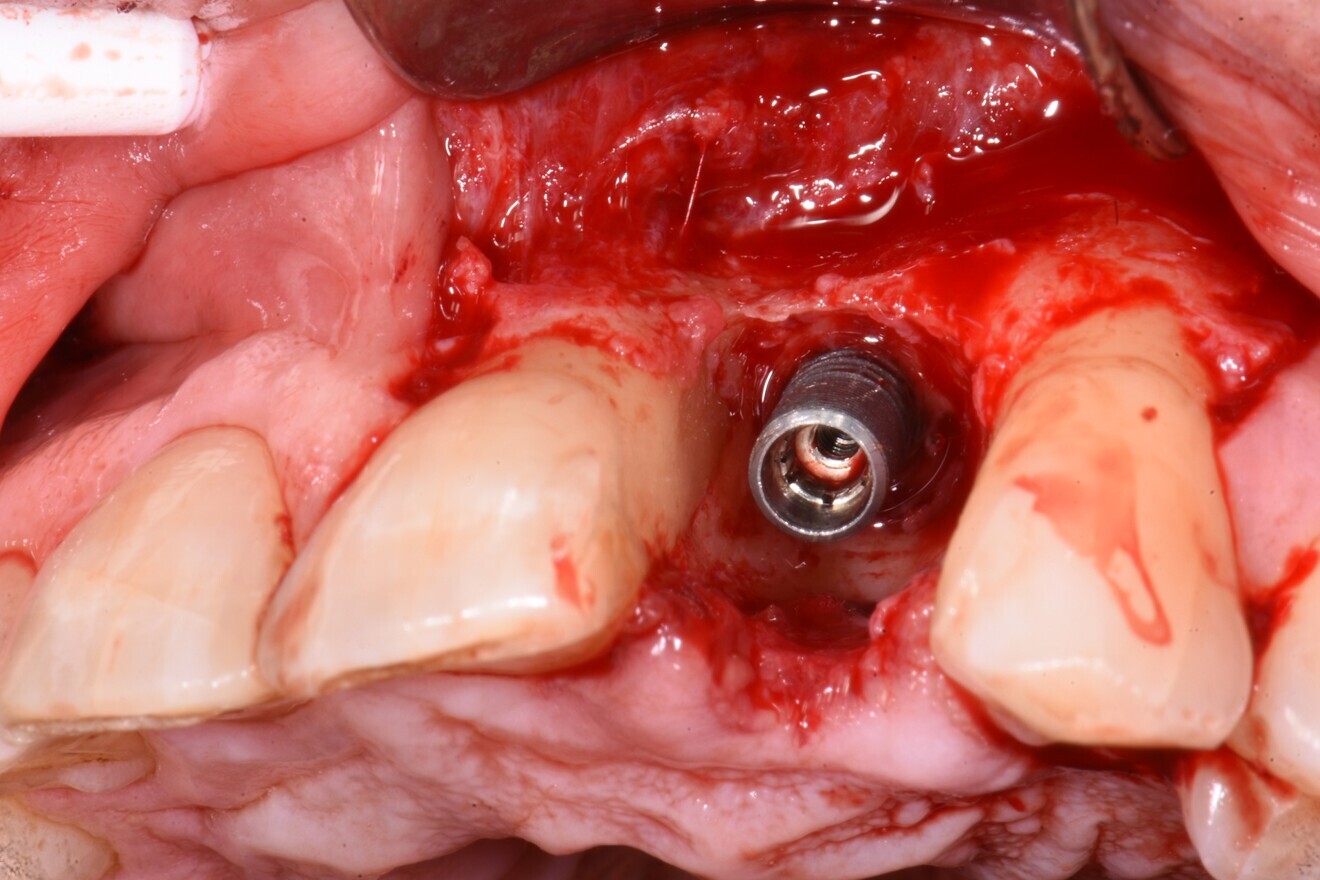
Tooth #11 was immobile and associated with adequate ridge width and a wide band of keratinised tissue (Fig. 1). There was also a favourable Class I incisor relationship and adequate space to accommodate an implant-supported restoration. A CBCT scan of the site revealed an inadequately endodontically treated tooth with a lack of an apical seal and incomplete obturation of the canal. The tooth benefited from good bone support provided by a robust facial bone plate at the alveolar crest (Fig. 2), but there was a large periapical dentigerous cyst measuring approximately 10 × 8 mm, extending to the mesial surface of tooth #12, and complete fenestration of the facial plate superiorly (Fig. 3). The prognosis of the tooth was deemed to be hopeless, and extraction was indicated.



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 International / International
International / International
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East
























































To post a reply please login or register